1801006120-Long Case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
A 55 year old male farmer by occupation resident of yadgirigutta came with chief complaints of
-deviation of mouth to left side since 7 days(11/3/2023)
-slurring of speech since 7 days
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptomatic 7 days ago then he had developed slurring of speech which was sudden in onset.On the same day his wife noticed deviation of mouth towards left side and was taken to local doctor for which he was given ORS but the symptoms has not subsided.
The next day his wife took him to another hospital for which he was given ORS.
On 13/3/2023 he came to our hospital.
At the time of presentation
Slurring of speech decreased
Slight deviation of mouth present
He is able to lift his hand, comb his hair, brush his teeth, able to wear his chappals, able to get up from bed
No history of vomiting,dizziness.
No history of blurring of vision
No history of drooling of saliva
No history of loss of consciousness
No drooping of eyelids
No history of difficulty in swallowing
PERSONAL HISTORY:-
Diet-mixed
Appetite-normal
Sleep-reduced
Bowel and bladder movements-regular
Addiction -no current addictions(used to drink sara 20 years back but he stopped later)
Daily routine:
Patient is a farmer by occupation resident of yadgirigutta.
Patient wakes up at 5am in the morning and does his daily work and prays for an hour.
He has rice for breakfast by 8 am.
He goes to the fields along with his wife on scooty by 9am.
He has his lunch by 1pm.
In the evening they return from work at 6pm.
He goes for bath and has his tea.
He has rice for dinner at 8pm and prays for an hour.
He goes to bed at 10pm
PAST HISTORY:
No historyof similar complaints in the past.
Known case of Tuberculosis 15 years back-used medication for 6 months
He is a known case of hypertension since 1 year and takes medicines irregularly(Tab.Amlodipine 5mg)
No history of diabetes,asthma,epilepsy.
FAMILY HISTORY:-
His father is a known case of of diabetes, hypertension and tuberculosis and he passed away due to covid.
Both his sisters are known case of diabetes and Hypertension.
Brother had history of stroke 3years ago.
GENERAL EXAMINATION:
Patient is conscious, coherant, cooperative,
moderately built and moderately nourished.
No pallor, icterus, cyanosis, clubbing, generalised edema or lymphadenopathy.
Vitals:
Temperature: afebrile
Pulse: 60 beats per minute
Blood pressure: 130/80 mmHg
Respiratory rate: 18 cycles per minute
Systemic examination:
CNS:
- Higher mental functions
conscious,coherent and cooperative
memory- able to recognize his family members
Speech - comprehension present, no fluency, repetition present
Cranial nerve examination
I- Olfactory nerve - sense of smell present
II- Optic nerve - visual acuity good
III- Oculomotor nerve, IV- Trochlear and VI- Abducens- no diplopia, nystagmus or ptosis
V- Trigeminal nerve- Masseter, temporalis and pterygoid muscles are normal. Corneal reflex is present.
VII- Facial nerve- face is symmetrical, forehead wrinkling present , nasolabial folds prominent on both sides.
VIII- Vestibulocochlear nerve- decreased hearing of the left ear ( rinne's test negative for 256 Hz and 512 Hz) and normal hearing of the right ear
IX- Glossopharyngeal nerve- palatal movements present and equal
X- Vagus- palatal movements present and equal
XI- Accessory nerve- sternocleidomastoid contraction present
XII- Hypoglossal nerve- deviation of tongue to right side and no fasciculations present
-Sensory system examination:
Right Left
crude touch Present Present
fine touch Present Present
pain Present Present
vibration Present Present
temperature Present Present
stereognosis Present Present
2 point discrimination Present Present
graphaesthesia Present Present
Motor system examination
BULK: Right Left
Upper limb Arm 28cm 29cm
Forearm 27 cm 26cm
Lower limb Thigh 49cm 49cm
Leg 33cm 31cm
TONE:
Upper limb Normal Normal
Lower limb Normal Normal
Right Left
POWER:
Upper limb hand 5/5 5/5
elbow 5/5 5/5
shoulder 5/5 5/5
Lower limb
- hip 5/5 5/5
- knee 5/5 5/5
- ankle 5/5 5/5
Right Left
REFLEXES: Biceps ++ ++
Triceps ++ ++
Knee +++ +++
Ankle + +
CARDIOVASCULAR SYSTEM:
Inspection :
No engorged veins, scars, visible pulsations
Palpation :
Apex beat - palpable in 5th inter costal space medial to mid clavicular line
No thrills and parasternal heaves can be felt
Auscultation :
S1,S2 are heard
no murmurs
PER ABDOMEN:
Inspection:-Umbilicus - inverted
All quadrants moving equally with respiration
No scars, sinuses and engorged veins , visible pulsations
Palpation - soft, non-tender
no palpable spleen and liver
Percussion:Resonant
Auscultation- normal bowel sounds heard
RESPIRATORY SYSTEM:
Inspection:
Shape of the chest : elliptical
B/L symmetrical.Both sides moving equally with respiration
No scars, sinuses.
Palpation:
Trachea - central
Expansion of chest is symmetrical.
Auscultation:
B/L air entry present . Normal vesicular breath sounds heard.
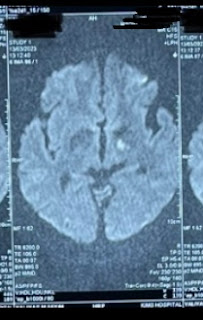
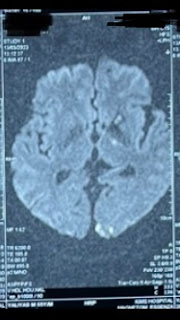
Provisional diagnosis:-
Acute Cerebrovascular accident involving left middle cerebral artery territory
Investigations:
Complete blood picture
Haemoglobin:11.7
Peripheral smear: normocytic normochromic anemia
Red blood cells:3.86
Platelet count:2.10
Total leucocyte count:5,100
Fasting blood sugar : 92 mg/dl
Serum creatinine :1.3 mg/dl
Blood urea 38 mg/dl
CUE:
Colour : pale yellow
Appearance : clear
Reaction :acidic
Albumin:nil
Sugar: nil
Bile salts and bile pigments : nil
RBC : nil
Crystals :nil
Casts : nil
pus cells:2-3
epithelial cells-2-3
Serum electrolytes
Sodium: 145 mEq/L
Potassium:4.2mEq/L
Chloride:104 mEq/L
Calcium ionized:1.11 mmol/L
MRI:-
X-ray chest










Comments
Post a Comment